A category of disorders known as Muscular Dystrophy lead to gradual muscle loss and weakening. The faulty genes (mutations) that cause muscular dystrophy prevent the body from producing the proteins required to develop healthy muscles. There are several types of muscular dystrophy. Symptoms of the most common type begin in childhood, mostly in boys. Other types do not surface until adulthood. There is no cure for muscular dystrophy. But medicines and treatments can help manage symptoms and slow the progression of the disease.

Understanding Duchenne Muscular Dystrophy
Progression of muscle weakening is the major sign of muscular dystrophy. Depending on the kind of muscular dystrophy, particular signs and symptoms appear at various ages and in various muscle groups. Here below are all the possible symptoms depending on the type of muscular dystrophy:-
1. Duchenne Type Muscular Dystrophy
This is the most common form. Although girls can be carriers and mildly affected, it is more common in boys. Signs and symptoms, which usually appear in childhood, may include:
- Frequent Falls
- Difficulty Rising from a seated or lying down posture
- Trouble running and jumping
- Wobbler
- Walking on toes
- Large muscles of the feet and calves
- Muscle pain and stiffness
- Learning Problems
- Delayed Growth
- Height Growth Problems
Read Also : Periodontitis (Gum Disease) – Being Trouble.
2. Becker Muscular Dystrophy
Its signs and symptoms are similar to those of Duchenne muscular dystrophy, but they are milder and progress more slowly. Symptoms usually begin in adolescence but may not occur until the mid-20s or later.

3. Oculopharyngeal Muscular Dystrophy (OPMD)
Oculopharyngeal Muscular Dystrophy (OPMD) causes weakness in the muscles of your face, neck, and shoulders. Other symptoms include:
- Fluttering Eyelids
- Eyesight problem
- Trouble swallowing
- Voice Change
- Heart problems
- Difficulty in walking
OPMD is one of the rarer types of muscular dystrophy, affecting less than 1 in 100,000 people in the United States. In their 40s or 50s, people typically start to exhibit symptoms.
4. Distal Muscular Dystrophy
Distal muscular dystrophy is also called Distal Myopathy. It is a group of more than six diseases that affect the muscles distal to the shoulders and hips, specifically:
- Forearms
- Hands
- Calves
- Feet
The respiratory system and cardiac muscles may also be impacted by the illness. Symptoms progress slowly and include loss of fine motor skills and difficulty walking. Distal muscular dystrophy symptoms typically appear in patients between the ages of 40 and 60.
What is Angina? Enemy of your heart?
5. Other Types of Muscular Dystrophy
Some forms of muscular dystrophy are distinguished by a particular trait or by the location of the onset of the symptoms in the body. Examples include the following:-
5.1 Myotonic
It is characterized by the inability of the muscles to relax after contraction. This form of muscular dystrophy causes myotonia, which is the inability of your muscles to relax after contracting. Steinert’s illness and dystrophia myotonica are other names for myotonic dystrophy. People with other types of muscular dystrophy do not experience myotonia, but it is a symptom of other muscle diseases. Symptoms include:
- Facial muscles
- Central Nervous System (CNS)
- Adrenal gland
- Heart
- Thyroid
- Eyes
- Gastrointestinal tract
Symptoms first appear in the face and neck. they include:
- Dropping of muscles in the face, creating a thin, drawn-out look
- Difficulty lifting the neck due to weak neck muscles
- Difficulty swallowing
- Drooping eyelids, or ptosis
- Early baldness in the frontal area of the scalp
- Poor vision including cataracts
- Weight Loss
- Increased sweating
Additionally, this form of dystrophy may result in testicular atrophy and impotence. In others, it can cause irregular periods and infertility.
Myotonic dystrophy is most likely to be diagnosed in adults in their 20s. The severity of symptoms can vary greatly. While some people only have minor symptoms, others may have heart- and lung-related problems that might be fatal. Many people with the condition live long lives.
5.2 Facioscapulohumeral (FSHD)
Muscle weakness usually begins in the face, hips, and shoulders. When the arms are raised, the shoulder blades can stick out like wings. Onset is usually in adolescence but can begin in childhood or as early as age 50.
5.3 Congenital
This type affects boys and girls and is evident at birth or before age 2. While some types evolve gradually and just slightly affect people, others advance quickly and seriously harm people.
Congenital muscular dystrophy is most often apparent between birth and 2 years of age. This is when parents begin to notice that their child’s motor function and muscle control are not developing as they should. Its symptoms vary and may include:-
- Muscle weakness
- Poor Motor Control
- Inability to stand or sit without assistance
- Scoliosis
- Foot deformity
- Trouble swallowing
- Respiratory problems
- Eyesight problem
- Speech Problems
- Learning Gaps
Symptoms range from mild to severe. The lifespan of a person with this type of muscular dystrophy also varies depending on their symptoms. Some people with congenital muscular dystrophy die in infancy, while others live to adulthood.
5.4 Limb-girdle
The muscles of the hip and shoulder are usually the first to be affected. People with this type of muscular dystrophy may have difficulty lifting the front part of the leg and may therefore trip frequently. Typically, onset starts in infancy or adolescence.
What is the Cause of Muscular Dystrophy?, Symptom Recognition, Treatment Options
Differences in genes cause muscular dystrophy. Thousands of genes are responsible for the proteins that determine the integrity of muscles. Humans carry genes on 23 pairs of chromosomes, with half of each pair inherited from biological parents.
One of these pairs of chromosomes is associated with sex. This implies that depending on your sex or the sex of your parents, the features or conditions you inherit as a result of those genes may vary. The other 22 pairs are not sex-linked and are also known as autosomal chromosomes.
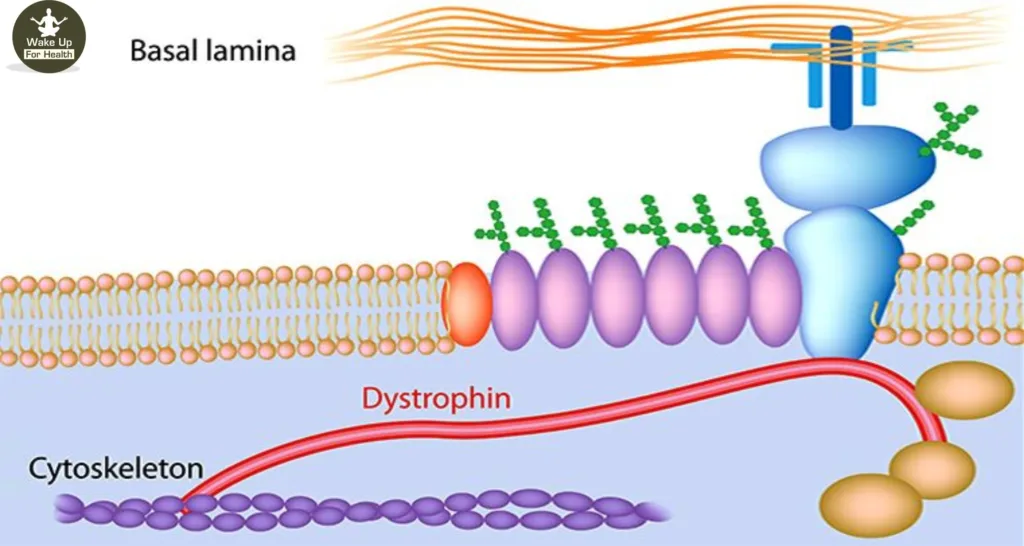
Changes in a single gene can result in a lack of dystrophin, an important protein. The body may not make enough dystrophin, may not make it correctly, or may not make it at all. There are four ways that people might get muscular dystrophy. The gene differences that cause muscular dystrophy are normally inherited, but they can also come from a spontaneous mutation.
What is the Treatment for Colorectal Cancer?
Risk Factors for Muscular Dystrophy?
Muscular dystrophy is a genetic condition. Being a carrier or getting muscular dystrophy is more likely if your family has a history of the disease. Since DMD and BMD are linked to the X chromosome, children who are assigned male are more likely to experience them.
However, even though children assigned to children receive one X chromosome from each parent and should have sufficient dystrophin production, they may still experience symptoms of DMD or BMD, such as muscle spasms, weakness. and heart problems.
What are the Complications of Muscular Dystrophy?

Complications of progressive muscle weakness include the following:
1. Difficulty walking. Some muscular dystrophies patients eventually use a wheelchair.
2. Trouble Using the Arms: Daily activities can become more difficult when the muscles of the hands and shoulders are affected.
3. Shortening of the Muscles or Tendons around the Joints (Contractures): Contractures can further limit mobility.
4. Difficulty in Breathing : Progressive weakness may affect the muscles involved in breathing. People with muscular dystrophy may eventually need to use a breathing assistance device (ventilator), initially at night but possibly during the day as well.
5. Curved Spine (Scoliosis) : Weak muscles may be unable to keep the spine straight.
6. Heart Problems :– Muscular dystrophy can reduce the functionality of the heart muscles.
Swallowing problems: If the muscles associated with swallowing are affected, nutritional problems and aspiration pneumonia may develop. Feeding tubes may be an option.
How to Diagnose Muscular Dystrophy?
Your doctor is likely to start with a medical history and physical exam. After that, your doctor may recommend some of the following tests:-
1. Enzyme Tests
Damaged muscles release enzymes like creatine kinase (CK) into your blood. In a person who has not suffered a traumatic injury, a high blood level of CK suggests muscle disease.
2. Genetic Testing
Blood samples can be tested for mutations in certain genes that cause the type of muscular dystrophy.
3. Muscle Biopsy
A small piece of muscle can be removed by making an incision or with a hollow needle. Analysis of tissue samples can differentiate muscular dystrophy from other muscle diseases.
4. Heart-Monitoring Tests (Electrocardiography and Echocardiogram)
These tests are used to check heart function, especially in people with myotonic muscular dystrophy.
5. Lung-Monitoring Tests
These tests are used to check the function of the lungs.
6. Electromyography
An electrode needle is inserted into the muscle for the test. The electrical activity is measured as you relax and gently tighten the muscles. Changes in the pattern of electrical activity can confirm muscle disease.
What is Treatment for Muscular Dystrophy?

There is currently no cure for muscular dystrophy, but treatments can help manage your symptoms and slow the progression of the disease. Treatments depend on your symptoms and the type of muscular dystrophy you have.
A. MEDICATIONS
For some DMD patients, new medicines have been authorised by the Food and Drug Administration (FDA). Many of these treatments use a new process called “exon skipping,” where the faulty section (exon) of the dystrophin gene is patched so that the body can produce the protein.
These new drugs include:
1. Eteplirsen (Exondys 51)
This weekly injection is for people with a specific mutation of the dystrophin gene that is responsible for skipping 51.
2. Golodirsen (Vyondys 53)
This weekly injection is for people who have dystrophin gene difference, which can lead to 53 skipping.
3. Viltolarsen (Viltepso)
It is also a weekly injection for people with dystrophin gene difference which is skippable by 53 skipping.
4. Deflazacort (Emflaza)
It is a corticosteroid which is available in tablet and oral suspension form. It is approved for people ages 5 and older with DMD.
B. MUSCLE THERAPY
Forms of muscle therapy have proven effective. These techniques include working with a professional to improve physical function. Types of therapy include the following:-
1. Physical therapy,
Including physical activity and stretching, to keep muscles strong and flexible
2. Respiratory Therapy
To prevent or delay breathing problems
3. Speech Therapy
Using specific techniques such as slow speech, pauses between breaths, and special equipment to preserve muscle strength.
(Disclaimer: This article is for general information only. It is just to wake you up for your health purpose. Out intension is not to mislead or It cannot in any way be a substitute for any medicine or treatment. Always contact your doctor for more details.)
2 thoughts on “Duchenne Muscular Dystrophy (DMD): Causes, Symptoms, Treatment”